How The Neck Affects The TMJ
Dr. Felix Periard • December 17th, 2023
Introduction
A Bit of TMJ Nomenclature...
TMJ: temporomandibular joint
Atlas/C1: first vertebra of the neck; sits under the skull
Axis/C2: second vertebra of the neck; sits under C1
Upper cervical spine: C1 and C2
Craniocervical junction: area comprised of the base of skull (cranium), the Atlas, and the Axis
Misalignment of the upper cervical spine = misalignment of the craniocervical junction = misalignment of the head and neck
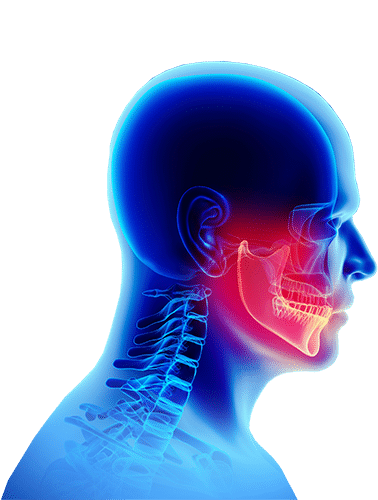
I rarely see a patient who hasn’t gone through a laundry list of professionals to get help with their temporomandibular joint (TMJ) dysfunction or temporomandibular dysfunction (TMD). It is also not uncommon to see patients with many associated symptoms such as headache, neck pain, tinnitus (ringing in the ear(s)), dizziness or vertigo, anxiety, etc. Even though there is a strong correlation between the neck and the jaw, very few are made aware of it. Indeed, your TMJ problem could be originating from your neck.
TMJ Discussion Points...
Nerves, Muscles, and Ligaments
The Connection Between the Neck & the TMJ
Let’s look to the nerve first.
The head, neck, and TMJ area are dense in nerves. The largest one, the trigeminal nerve is responsible for the sensory information of the head and face. This nerve originates from the brainstem (the transitional area between the brain and the spinal cord), which is located at the craniocervical area (the junction between the uppermost part of the cervical spine and the cranium). In addition, the third branch of the trigeminal nerve innervates the 4 muscles of mastication.
As described in this paper published in the journal BioMed Research International 1: “The possible explanation could be the neurophysiologic connections between the cervical spine and temporomandibular area, such as the convergence of trigeminal and upper cervical afferent inputs in the trigeminocervical nucleus.”
In our article “Non-Surgical Treatment of Trigeminal Neuralgia”, I discuss why we examine the structural integrity of the upper cervical spine and craniocervical junction. Here I write:
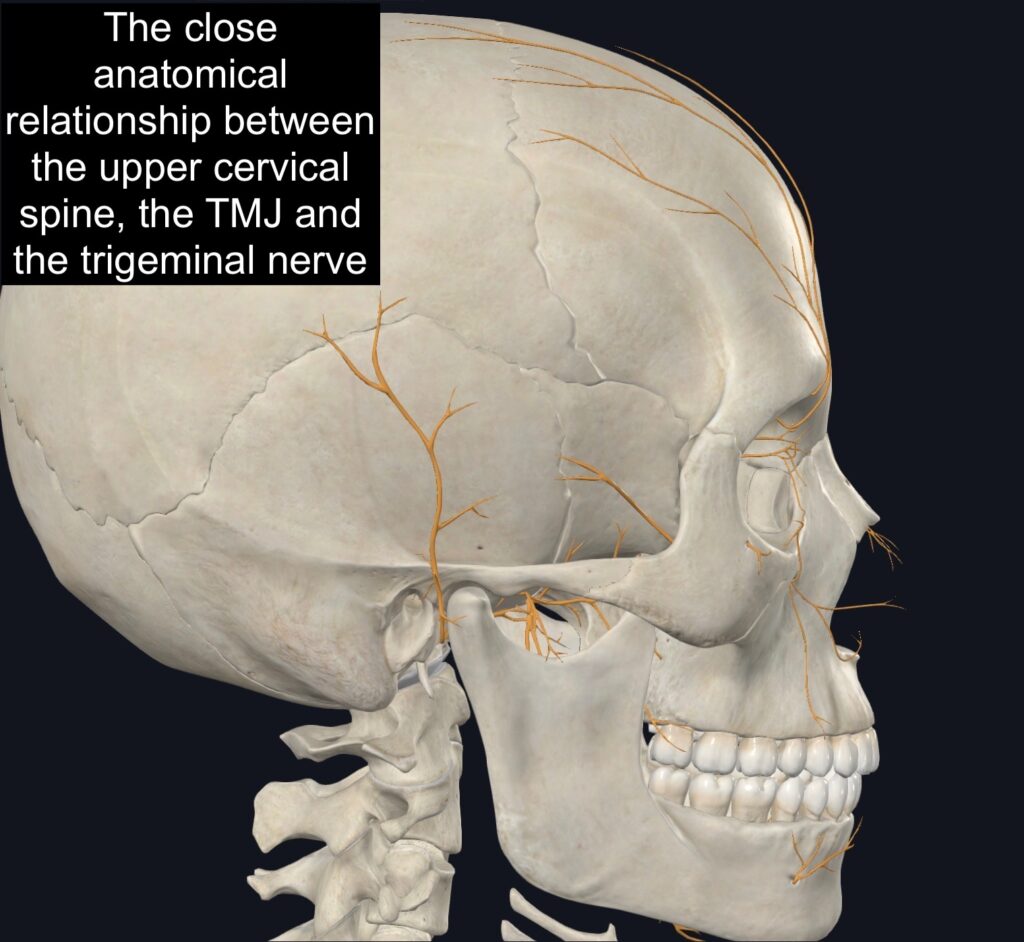
We evaluate the head and neck of patients suffering from trigeminal neuralgia because we are looking for indications of compression of the nerve and misalignment of the Atlas (C1), the neck, and the head. The head and neck have a rather unstable relationship and I commonly see structural issues with this area in patients suffering from trigeminal neuralgia. Because of the close link between the neck and the jaw, one can cause issues to the other and vice versa. Plus, any problem with the neck can cause different neuralgia such as trigeminal neuralgia and occipital neuralgia.
When a surgeon believes there is a compressed nerve it makes sense why they would want to do surgery to decompress the nerve. However, if the compression problem comes from an issue with the alignment of the spine, the surgery won’t help fix this misalignment and the pain won’t disappear.
It’s also important to note that a problem with the alignment of the cervical spine (neck spine) is the most common cause of all types of headaches and migraines.
This has been known for a very long time hence why our evaluation always begins with a careful analysis of our patient’s head and neck.
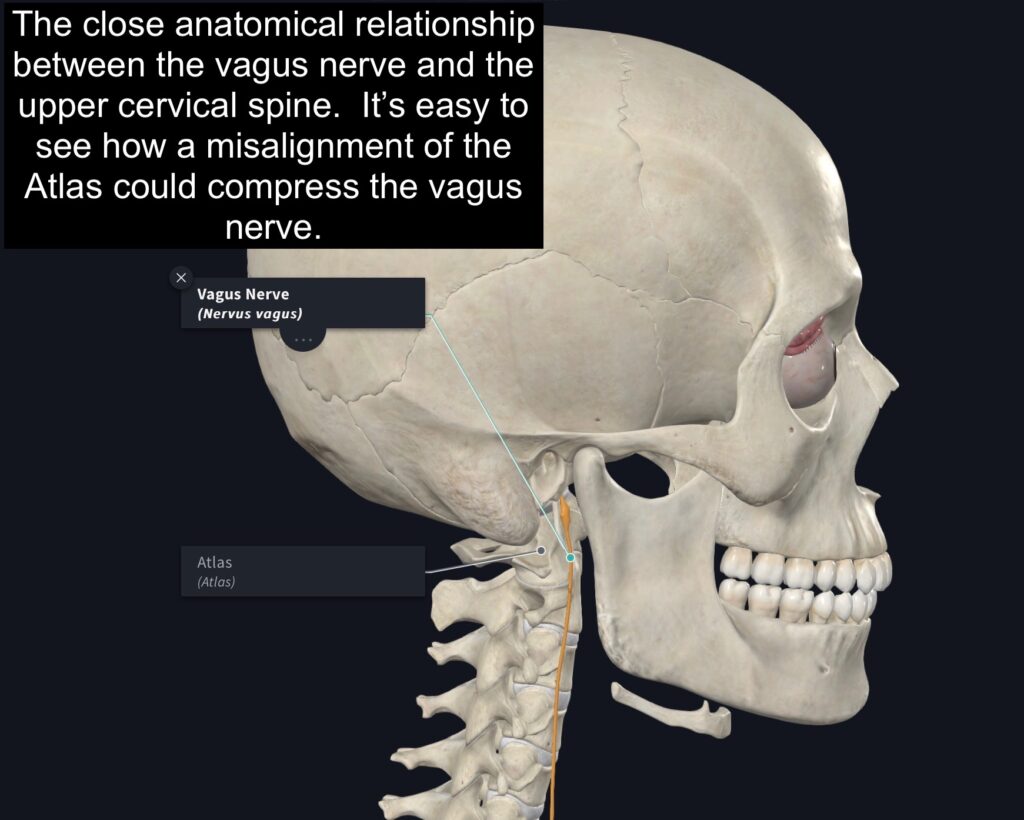
Back to the nerves of the head, neck, and jaw. I must also stress the close relationship between the vagus nerve and the neck. The vagus nerve travels down in front of the Atlas (C1). In some patients with serious rotational misalignment of their Atlas, mechanical compression of the vagus nerve is likely. This will result in a disruption of the parasympathetic tone of the nervous system; the vagus nerve being the most important parasympathetic nerve of the human body.
The parasympathetic branch of the nervous system is responsible for calming and quieting the body. A compressed vagus nerve will alter this function and lead to an increase in sympathetic tone; which is responsible for energizing and heightening senses. After being “stuck” in sympathetic mode for a while, muscles become very tense and tight; muscles of the jaw being amongst the most commonly affected (along the the trapezius and low back muscles). This increase in tensing can lead to clenching, aggravating the TMJ dysfunctions.
Let’s stop here for a recap.
- The trigeminal and vagus nerve can both affect the TMJs.
- The trigeminal nerve is responsible for pain sensation and mastication muscle innervation.
- The vagus nerve is responsible for the calm and restful state of the body.
- A misalignment of the spine can cause compression on either or both nerves leading to dysfunction, pain, and tension.
Now let’s look at the muscles.
As discussed above, the third branch of the trigeminal nerve innervates the 4 muscles of mastication (masseter, temporalis, medial and lateral pterygoid).
In 2017, researchers from the University of Comenius’ Faculty of Medicine in Slovakia 2, found that: “Wrong body position in combination with spinal root compression and implicated prolonged isometric contraction of the muscles and other degenerative changes in tendons and ligaments are the most important etiologic factors of the disorder. The formation of myofascial pain in the head and neck is significantly influenced by hyperextension of the upper cervical spine (C1–C3) and flexion of its lower part (C4–C7) .”
They concluded by writing: “A long-term cervical dysfunction can influence the function of masticatory muscles and TMJ.”
A paper published in the Journal of Oral Surgery and Maxillofacial Surgery 3, in 2020, found that: “altered head and neck posture and FHP (Forward Head Posture) showed an association between the onset of sustained strain in the masticatory and cervical muscles.”
Once again, we see a strong correlation between the cervical spine and the jaw. This article also points to a very important problem and a major factor in TMJ dysfunction: hyperextension of the upper cervical spine (C1-C3 ) and flexion of its lower part (C4-C7). This translates to a loss of the normal cervical curvature (lordosis); also coined FHP because the head is forward as compared to where it should naturally sit: over the shoulders. A straight neck or reversed curvature are problems I see in just about all patients suffering from TMJ dysfunction. We will dive deeper into this issue and its link to TMJ dysfunction a little later in the article.
Finally, let’s take a peek at the ligaments.
Keeping with the subject of FHP for just an instant. When the head rests in a forward position, with time, this passive tension will pull on the infra- and supra-hyoid muscles causing the mandible (jaw bone) to move downward and backward. This changes the position of the condyles (the part of the mandible that attaches to the cranium) backward. This forces the lateral pterygoid muscles to work overtime as their job is to bring the jaw forward. This time, this constant tension on muscles and backward moving of the jaw causes the lateral temporomandibular ligaments to overstretch; resulting in TMJ instability.
This is the chain of events:
- An abnormal position of the head and neck causes pressure and dysfunction on nerves AND tension in the muscles of the neck and jaw muscles
- This alters the normal position of the jaw, causes a lot of tightness in the mastication muscles, and pain to the face
- A posterior (backward) positioned jaw causes abnormal tension on the lateral temporomandibular ligaments; creating TMJ instability
Forward Head Posture (FHP) and TMJ Dysfunction
As pointed out by this paper published in the Journal of Orofacial Pain 4: “studies have reported the position of the head affects the resting position of the mandible, increases muscular activity, and alters the internal arrangement of the TMJ. In addition, a close association between head and cervical posture improvement and the relief of symptoms of TMD has been found.”
They concluded by writing: “an abnormal head and cervical posture was present in patients with TMD” and “lower lordosis angle in patients with TMJ internal derangement determined with MRI compared with controls who had normal disc position, determined by MRI as well.”
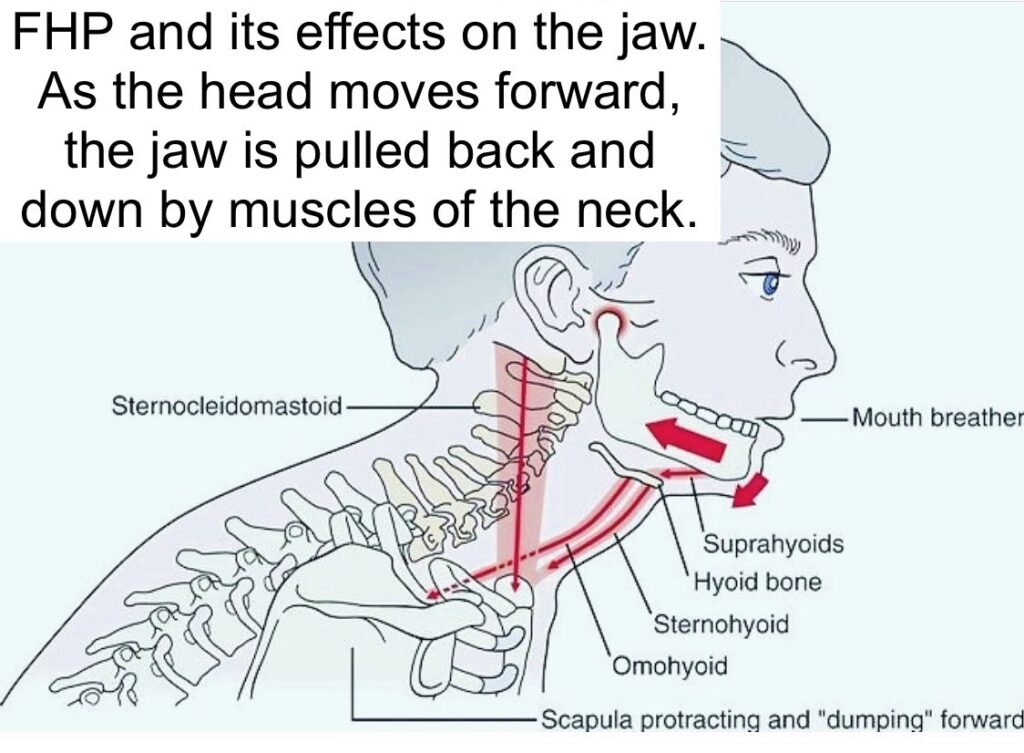
In our article “The Consequences of a Misaligned Head and Neck on Airway Dimensions and Sleep Apnea”, I discuss the further repercussions that FHP has on airway dimensions and how it can cause breathing problems such as sleep apnea. Here I write:
A paper published in (Associations Among Temporomandibular Joint Osteoarthritis, Airway Dimensions, and Head and Neck Posture) reports many interesting facts when it comes to airway dimension, TMJ dysfunction, and FHP. “A small retruded mandible seems to show interactions with decreased pharyngeal airway volume.” They also write: “Retrognathic (a retracted/backward jaw) facial profiles may exhibit decreased airway dimensions and altered head and neck posture and FHP showed an association between the onset of sustained strain in the masticatory and cervical muscles.”
They also discovered that a backward positioned jaw and a large craniocervical angle (an indication of FHP) were more frequent in patients with TMJ OA (osteoarthritis).
Neck Pain & Asymptomatic
Temporomandibular Dysfunction
Going back to the paper published in 2021 in the journal BioMed Research International 1. The research article ends with this conclusion: “The results of our research allow to suggest that idiopathic neck pain is associated with limited range of motion in the cervical spine, incorrect head posture, and dysfunction of TMJ. This study may indicate that therapy focusing only on the cervical region could improve clinical condition of TMJ in subjects with idiopathic neck pain but not reporting TMJ pain.”
They also point out that “In our study, we found more cases of TMDs in participants with neck pain than in pain-free control participants.” Also, “In our research, 76% of the experimental group demonstrated forward head posture compared to only 20% in the control group.”
This all brings us back to the effects of the neck on the function of the TMJ and all those joints involved. Neck pain is usually one of the first symptoms of a problem with the cervical spine. Whether TMJ pain is present or not at that moment, prolonged dysfunction of the cervical spine could likely lead to TMJ dysfunction.
This article brings us to another very important discussion point: the lack of mobility at the upper cervical area and its connection to TMJ dysfunction.
Decreased Mobility at the Upper Cervical Spine
We have now looked at nerves, muscles, ligaments, and head position as it relates to TMJ dysfunction. We also know neck pain is very common in people with OR without TMJ dysfunction.
Let’s now look at the connection between mobility, or lack of, at the upper cervical area and TMJ dysfunction.
An article published in the European Journal of Oral Sciences 5, in 2020, stated “Patients in the pain-related and mixed TMD groups were found to have decreased upper neck mobility in the cervical flexion-rotation test compared with patients in intra-articular and control groups, as well as poorer capabilities of the deep neck flexor muscles in the craniocervical flexion test compared to the control group.”
The cervical flexion-rotation test is used to isolate and test the range of motion between the Atlas (C1) and the Axis (C2), commonly known as the upper cervical vertebrae.
In another article published in the Journal of Oral Rehabilitation 6, in 2019, looking at headaches, TMD, and cervical spine dysfunction, researchers concluded that: “Women with TMDs, regardless of self-reported headaches, showed limited flexion/extension ROM, limited upper cervical spine (C1-C2) mobility and poor deep cervical flexor performance.”
This conclusion not only reinforces the issue with the upper cervical spine mobility but also with FHP. Someone with FHP will show, more often than not, a decrease in deep cervical flexor muscle strength. The deep flexors are responsible, as the name implies, for flexing (more so retracting in their case) the neck.
Headaches are commonly associated with TMD. A paper published in the Journal of Craniomandibular and Sleep Practice 7, in 2014, concluded that “Subjects with TMD had signs of upper cervical spine movement impairment, greater in those with headache.”
Finally, an article published in the Journal of Clinical Oral Investigations 8, in 1998, concluded that “The results indicated that segmental limitations (especially at the C0-C3 levels) and tender points (especially in the m. sternocleidomastoideus and m. trapezius) are significantly more present in patients than in controls.”
Let’s stop here for a recap.
- Multiple researchers found a connection between TMD and a lack of range of motion at the upper cervical spine
- There is a connection between a decreased range of motion of the upper cervical spine, TMD, and headaches
- Patients with TMD have a decrease in deep flexor muscle strength
Let’s look at one last article diving into the link between upper cervical motion and jaw motion. This last article studied the connection between jaw motion, neck motion and muscle activation. The paper opens with this statement: “Most species exhibit a wide range of head-neck movements in activities that are influenced or initiated by input from oro-facial structures (Abrahams et al., 1993), indicating that movement of the head is an integral part of normal oral function.” Published in 2020 in the Journal of Dental Research 9, the paper concluded by saying “Taken together, evidence from our previous and present studies shows that jaw-opening/-closing movements during natural jaw activities are not dependent on only mandibular movements in relation to the cranium. We, therefore, suggest a new concept for human jaw function, in which “functional jaw movements” are the result of coordinated activation of the jaw as well as neck muscles, leading to simultaneous movements in the temporomandibular, atlanto-occipital, and cervical spine joints.”
We now have a final link between the normal movement of the jaw and the upper cervical spine.
A lack of motion in the upper cervical is synonymous with misalignment.
A lack of mobility, in most cases, indicates a bigger problem. This problem is misalignment. The upper cervical spine has a unique role in our survival. The first vertebra (C1), the Atlas, being shaped like a donut, articulates on top of C2, the Axis. The Axis has a peg around which the Atlas can rotate giving us an incredible range of motion and allowing us to look around. Most of the rotation in the neck comes from the C1/C2 junction. In addition, the skull lazily sits on top of the Atlas. It rocks forward and backward allowing us to look up and down. All this phenomenal range of motion comes at a price, and this price is named “instability.” Compared to all other joints of the spine, the upper cervical area has no locking mechanism. What I mean by this is the skull is floating on top of the Atlas and the Atlas on top of the Axis. All that is holding these structures together are ligaments.
This instability is also what permits the Atlas to move out of alignment and get stuck like that. A misaligned Atlas will always result in a decrease of range of motion as the joints cannot glide and slide like they should.
How the Upper Cervical Spine Affects Occlusion
Based on everything we have visited so far, I believe it is safe to assume the intricate connection between the neck and the TMJs. Occlusion (how the teeth close together a.k.a. bite) plays a big role in possible future TMJ dysfunction; an uneven bite creates uneven stress on the TMJs.
Although biting is a pretty menial task, it can have repercussions in other areas than the jaw. The forces created by biting down are significant and in the event where the occlusion is not equal and even, these forces will be transmitted to the TMJs, but also to the spine. Adding to that the imbalance in masticatory muscles resulting from a misaligned neck and you have a perfect recipe to end up with TMD.
Before we explore different research articles, I want to establish the link between the neck, global posture, and functional leg length asymmetry. Functional leg length asymmetry refers to the phenomenon where a leg “appears” shorter when compared to the other one. It is not a bone problem, per se, but a muscle problem. What I mean by this is: the bones of the leg are not short, but some muscles in the back or hip are pulling the one leg up, creating the image of shortness.
This happens when there is an imbalance in the contraction of muscles, right compared to left. This imbalance will also result in a shift in normal posture. These changes result most often from a misalignment of the upper cervical spine.
The reticular formation is a special bundle of nerves hidden and protected by the Atlas (C1), the top bone of the spine. This formation’s role is to control the anti-gravity muscles, namely the muscles of the back keeping us upright and straight. A misalignment of the upper spine (head, Atlas and Axis) causes dysfunction of this bundle of nerves resulting in increased contraction on one side of the back and hips and a decrease on the opposite side. As you can probably imagine, this produces a functional short leg.
Now that this has been demonstrated, let’s take a look at the effect of occlusal alteration and masticatory imbalance on the cervical spine.
In an article published in 2003 in the European Journal of Orthodontics 10, researchers write “In the cervical spine, high stress was observed at C1, suggesting its importance in maintaining posture.”
Using a computer-generated 3D model of the human body, these doctors evaluated the effects of abnormal occlusal plane and/or masticatory muscle tension on the cervical spine.
An increase in muscle strength/tension created an increase on the cervical spine stress on the same side and a deviation of the spine on the opposite side. Similarly, a shift and elevation of the occlusal plane created same-side stress on the cervical spine and an opposite-side deviation.
Let’s recap here for a second:
- The cervical spine, especially the upper cervical spine is intricately connected to posture and unequal leg length
- A shift and misalignment of the upper cervical spine creates abnormal posture and a functional short-leg
- Unequal masticatory muscle tension/strength and/or uneven occlusal plane will create abnormal stress and deviation of the cervical spine
Let’s now dive into the effects of a short leg on the TMJs.
A paper published in the Journal of Craniomandibular & Sleep Practice 11, in 2011, reported the effects of a functional short leg on dental occlusion. Researchers experimentally created a short leg (or long leg) in the subjects by using insoles with heel lifts of different heights. They concluded that “When subjects used a heel lift of eight mm or more under the right foot, occlusal force shifted to the right side compared to the control (p<0.05). When subjects used a heel lift of seven mm or more under the left foot, occlusal force shifted to the left side compared to the control (p<0.05).”
Abnormal occlusion will end up creating uneven wear and tear on the TMJs and lead to TMD. It will also create unequal stress on the spine and accentuate the already present misalignment of the neck, worsening the state of imbalance between the head, neck, and TMJs. This vicious circle will keep on repeating itself until both issues, the neck and the TMD, are addressed
Summary
It comes with very little surprise that the TMJs and the neck have a significant connection. The vagus nerve and trigeminal nerve play an important role in innervating the masticatory muscles and sending pain signals from the face. These nerves are easily and often affected by a misalignment of the upper neck. Such misalignment invariably comes with a shift in the center of gravity and FHP. FHP has a myriad of effects on the TMJ: it will alter normal muscle tension and TMJ biomechanics by shifting the jaw backward and downwards. This will in turn create an increased stress on the lateral temporomandibular ligament.
People suffering from TMJ dysfunction (or TMD) are much more likely to have decreased upper cervical spine ranges of motion. This was also linked to more prevalent headaches. A misaligned joint, whether vertebral or not, will always be a joint that lacks a normal range of motion.
Finally, malocclusion causes abnormal stress on the spine which results in its lateral deviation. This accentuates the already present misalignment issue. An issue that causes an uneven leg length that further affects the TMJ and occlusion.
TMJ Dysfunction Treatment
Per the recommendation of The National Institute of Dental and Craniofacial Research, a branch of the US government’s National Institutes of Health, it is important to take precautions in treating TMJ disorders. They recommend that patients avoid treatments that cause permanent changes to the jaw joint, teeth or bite; or surgery. Such treatments include crown and bridgework to equalize occlusion, orthodontics to change teeth alignment, and grinding down teeth to bring the bite into balance (occlusal adjustment).
TMJ dysfunction (or TMD) is a dual problem, in my opinion. Meaning 2 issues must be addressed:
- the upper cervical misalignment and
- the occlusion
The upper cervical misalignment correction is our specialty.
We evaluate the head and neck of patients suffering from TMJ dysfunction because we are looking for indications of misalignment of the Atlas (C1), the neck, and the head. The head and neck have a rather unstable relationship and I commonly see structural issues with this area in patients suffering from dysfunction. Because of the close link between the neck and the jaw, one can cause issues to the other and vice versa.
When a dentist wants to fix a malocclusion problem it makes sense. Some occlusion treatments, that are gradual and reversible, can be extremely beneficial. However, many patients will only find partial relief from such a procedure until the problem with the alignment of their neck is resolved.
It’s also important to note that a problem with the alignment of the cervical spine (neck spine) is a common cause of all types of headaches including migraine, tension-type, cervicogenic, cluster, and thunderclap.
This has been known for a very long time hence why our evaluation always begins with a careful analysis of our patient’s head and neck.
If you’re interested in having your own evaluation, you can schedule a consultation with Dr. Felix Periard with the button below!
References
- Oleksy Ł, Kielnar R, Mika A, Jankowicz-Szymańska A, Bylina D, Sołtan J, Pruszczyński B, Stolarczyk A, Królikowska A. Impact of Cervical Spine Rehabilitation on Temporomandibular Joint Functioning in Patients with Idiopathic Neck Pain. Biomed Res Int. 2021 Oct 7;2021:6886373. doi: 10.1155/2021/6886373. PMID: 34660797; PMCID: PMC8516540.
- Halmova K, Holly D, Stanko P. The influence of cranio-cervical rehabilitation in patients with myofascial temporomandibular pain disorders. Bratisl Lek Listy. 2017;118(11):710-713. doi: 10.4149/BLL_2017_134. PMID: 29216730.
- Kang JH. Associations Among Temporomandibular Joint Osteoarthritis, Airway Dimensions, and Head and Neck Posture. J Oral Maxillofac Surg. 2020 Dec;78(12):2183.e1-2183.e12. doi: 10.1016/j.joms.2020.08.006. Epub 2020 Aug 12. PMID: 32898485.
- Olivo SA, Bravo J, Magee DJ, Thie NM, Major PW, Flores-Mir C. The association between head and cervical posture and temporomandibular disorders: a systematic review. J Orofac Pain. 2006 Winter;20(1):9-23. PMID: 16483016.
- Greenbaum T, Dvir Z, Emodi-Perelmam A, Reiter S, Rubin P, Winocur E. Relationship between specific temporomandibular disorders and impaired upper neck performance. Eur J Oral Sci. 2020 Aug;128(4):292-298. doi: 10.1111/eos.12718. Epub 2020 Jul 6. PMID: 32627243.
- Ferreira MP, Waisberg CB, Conti PCR, Bevilaqua-Grossi D. Mobility of the upper cervical spine and muscle performance of the deep flexors in women with temporomandibular disorders. J Oral Rehabil. 2019 Dec;46(12):1177-1184. doi: 10.1111/joor.12858. Epub 2019 Aug 1. PMID: 31292981.
- Grondin F, Hall T, Laurentjoye M, Ella B. Upper cervical range of motion is impaired in patients with temporomandibular disorders. Cranio. 2015 Apr;33(2):91-9. doi: 10.1179/0886963414Z.00000000053. Epub 2014 May 23. PMID: 25919749.
- De Laat A, Meuleman H, Stevens A, Verbeke G. Correlation between cervical spine and temporomandibular disorders. Clin Oral Investig. 1998 Jun;2(2):54-7. doi: 10.1007/s007840050045. PMID: 15490776.
- Eriksson PO, Häggman-Henrikson B, Nordh E, Zafar H. Co-ordinated mandibular and head-neck movements during rhythmic jaw activities in man. J Dent Res. 2000 Jun;79(6):1378-84. doi: 10.1177/00220345000790060501. PMID: 10890716.
- Shimazaki T, Motoyoshi M, Hosoi K, Namura S. The effect of occlusal alteration and masticatory imbalance on the cervical spine. Eur J Orthod. 2003 Oct;25(5):457-63. doi: 10.1093/ejo/25.5.457. PMID: 14609013.
- Maeda N, Sakaguchi K, Mehta NR, Abdallah EF, Forgione AG, Yokoyama A. Effects of experimental leg length discrepancies on body posture and dental occlusion. Cranio. 2011 Jul;29(3):194-203. doi: 10.1179/crn.2011.028. PMID: 22586828.
