Headache? Probably a Neck Problem
Dr. Felix Periard • January 7th, 2024
Introduction
A Bit of Headache Nomenclature...
Headache: pain or discomfort in the head or face area
Atlas/C1: first vertebra of the neck; sits under the skull
Axis/C2: second vertebra of the neck; sits under C1
Upper cervical spine: C1 and C2
Craniocervical junction: area comprised of the base of skull (cranium), the Atlas, and the Axis
Misalignment of the upper cervical spine = misalignment of the craniocervical junction = misalignment of the head and neck
There are dozens of headache diagnoses: cervicogenic, tension, sinus, migraine, cluster, chronic, etc. Patients stepping through our doors are usually confused more than they’ve ever been; they have seen a laundry list of professionals and have had more tests and scans done than a cancer patient and yet, nothing.
There are dozens of headache diagnoses: cervicogenic, tension, sinus, migraine, cluster, chronic, etc. Patients stepping through our doors are usually confused more than they’ve ever been; they have seen a laundry list of professionals and have had more tests and scans done than a cancer patient and yet, nothing.
Tests show nothing. Scans show nothing. The brain looks ok. The cervical spine looks ok…maybe a bit of degeneration (arthritis) but that’s it.
Most will point to a problem with their neck in addition to their headache. We often hear “My head feels very heavy, almost impossible to keep up.” or “I always feel tension at the base of my skull…I feel like my headache stems from this area.” Some will also straight up state that the pain starts in their neck a travels to their head.
Although all tests or scans are negative, something has to be wrong, otherwise there would be no headache.
All sorts of pains are signals your body uses to alert you to a danger or something malfunctioning. In the event of headaches, it is something malfunctioning, in 95% of cases.
Where does this malfunction stem from, then?
The neck. More than 90% of headaches stem from a dysfunction of the craniocervical (upper neck)/cervical (neck) area 1. Let me repeat that: 90% of headaches stem from the neck or upper neck. Some uncommon headaches are due to a problem in the brain or blood vessels. Sinus infection can also cause headaches, but those are few and far between.
Headache Discussion Points...
Anatomy of Headache
Before we dive into the intricate links between the neck and head and how they relate to headaches, we will take a look at some basic anatomy to better understand where they stem from and why they happen.
First, it is vital to understand that all head and face pain is perceived by nerves originating from the neck. The trigeminal nucleus, located in the brainstem, is a small bundle of nerve fibers receiving nociceptive (pain) input from the head and face area. The brainstem is the junction between the brain and spinal cord; it is found, encased by the Atlas, the first vertebra of the neck, and the Foramen Magnum (the hole at the bottom of the skull through which the brain descends). This particular area of the spine is known as the craniocervical junction.
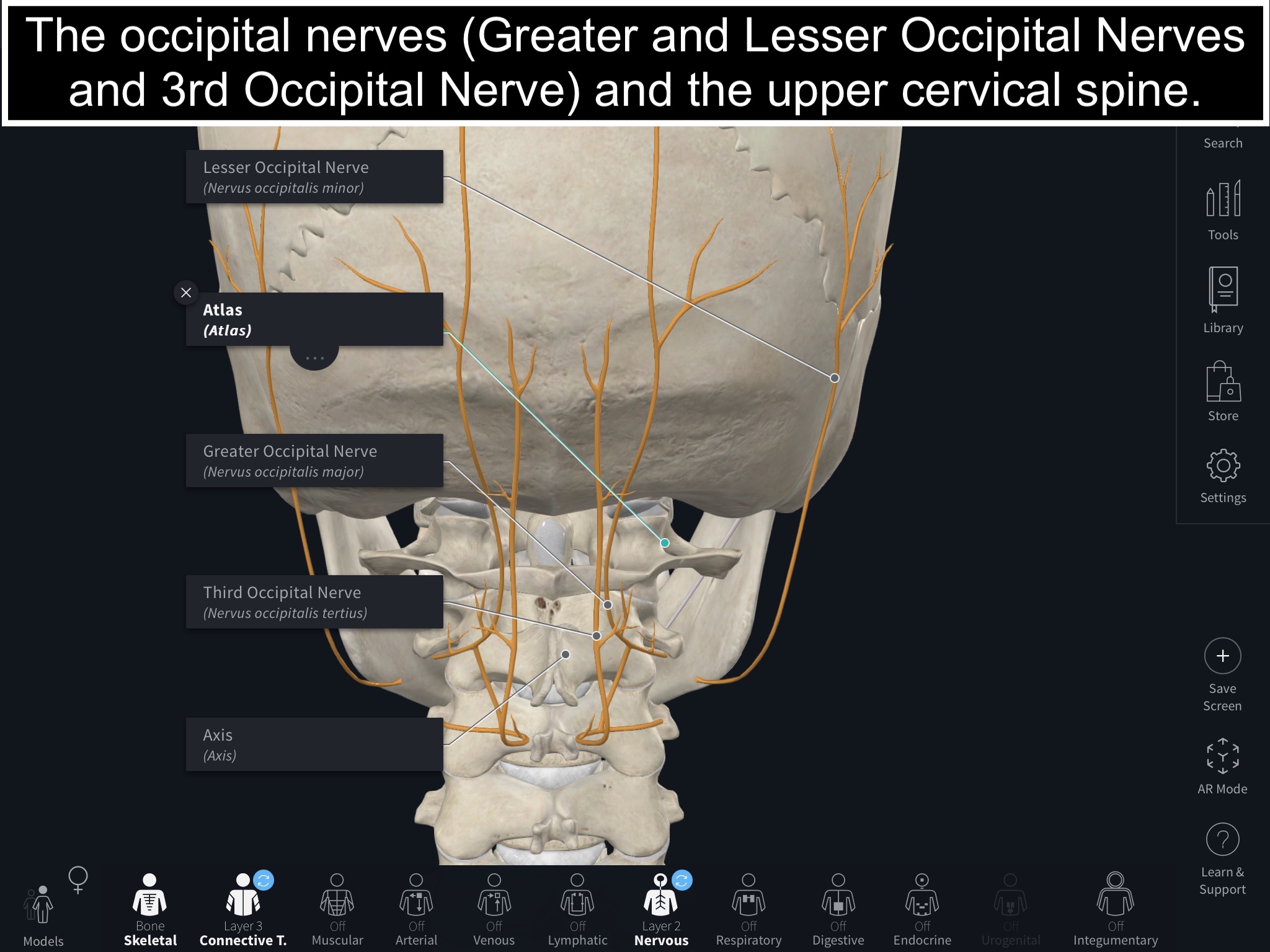
The upper cervical afferents (nerves receiving information, rather than sending), originating from nerve roots from the C1, C2, and C3 cervical vertebrae, also perceive nociception (pain). These nerves travel from the upper cervical levels to the back of the head. They are the main culprits of occipital neuralgia, for example.
Let’s stop here for a recap.
- All head and face pain is perceived by the trigeminal nucleus
- The trigeminal nucleus is located at the craniocervical junction; encased by the Atlas and Foramen Magnum
- Special nerves originating from the upper cervical vertebrae receive pain sensation from the back of the neck and head
The spine is made up of 24 mobile segments called vertebrae. Each vertebra (except the top and bottom one) articulates with the one above and the one below; meaning, vertebrae have joints that allow them a certain freedom of movement. The Atlas articulates with the base of the skull, above; and the last lumbar (low back) vertebra articulates with the sacrum, under.
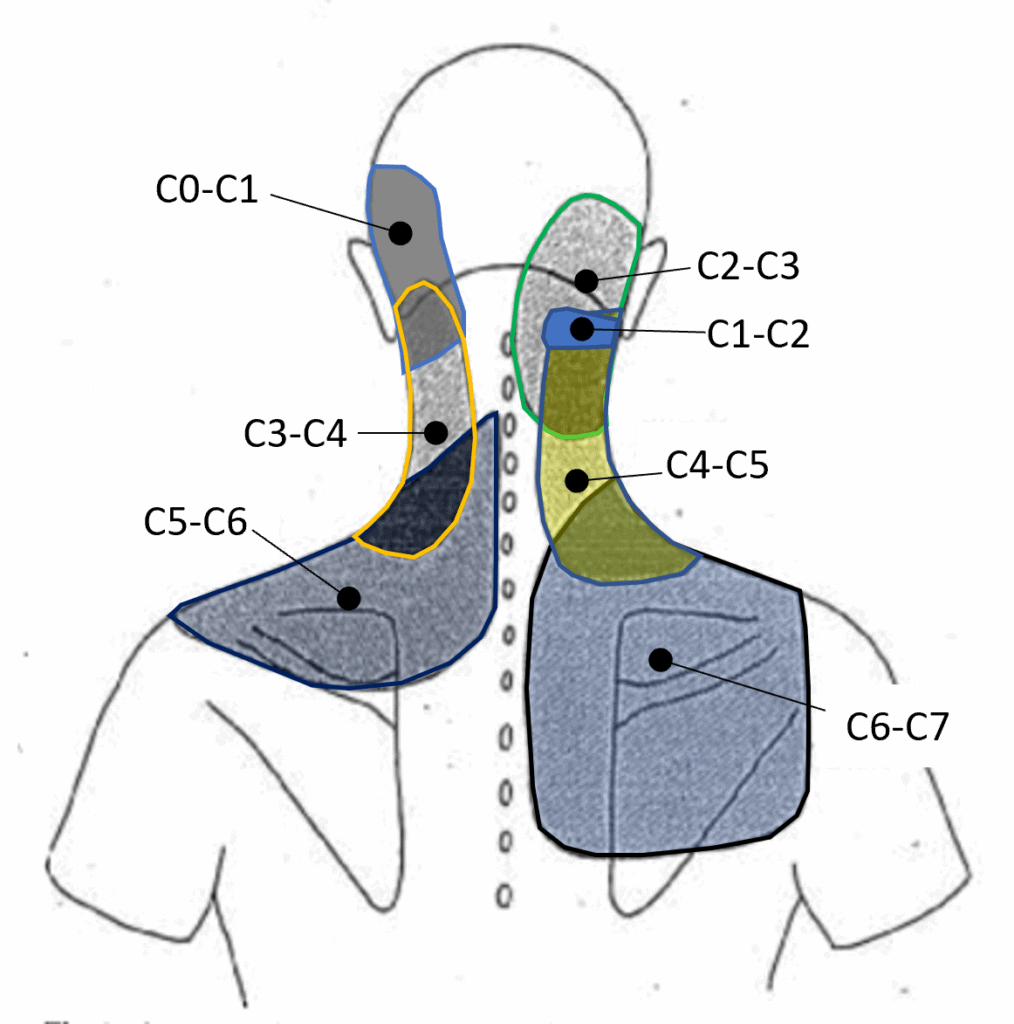
Different joints of the spine can cause different pain patterns, also known as referral patterns.
As you can see in this image, different joints of the spine can cause referred pain to the head; especially C0 (occiput — base of the skull) to C3.
In some cases, those joints are damaged and arthritic and they require the attention of a medical doctor who can do the appropriate regenerative medicine injection (such as prolotherapy, PRP, or stem cells).
Ligament instability can also be a cause of neck pain and lead to early onset of arthritis.
However, in some other cases, the problem is purely mechanical. What I mean by this is that the joints are not properly aligned and moving like they need to. This causes friction and irritation which is the source of pain.
Lastly, let’s talk about muscles for a bit. There are a multitude of muscles attaching to the spine and skull. Just like all, they create motion by contracting. The problem resides in the fact that sometimes a muscle will go into spasm (hyper-contraction) and not let go.
This is often due to the muscle attempting to:
- Stabilize an unstable structure (joint)
- Reposition something misaligned
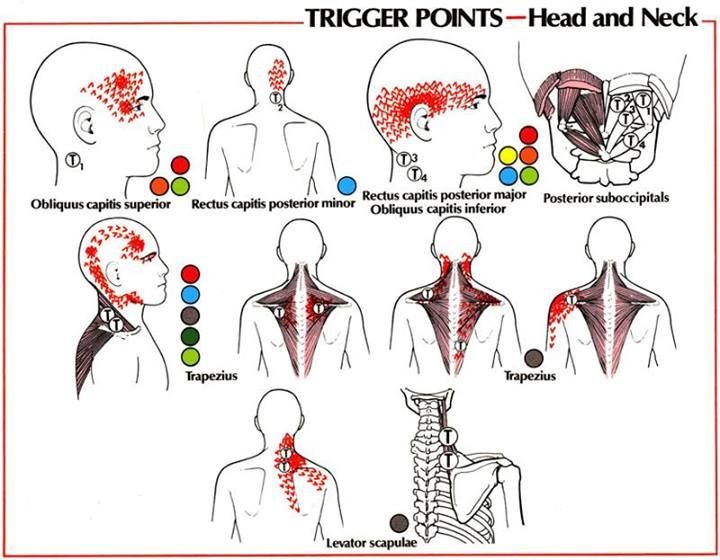
If these spasms do not disappear, trigger points form.
Authors described trigger points in an article published in the American Family Physician journal 2: “Trigger points are discrete, focal, hyperirritable spots located in a taut band of skeletal muscle. They produce pain locally and in a referred pattern and often accompany chronic musculoskeletal disorders. […] These include muscles used to maintain body posture, such as those in the neck, shoulders, and pelvic girdle. Trigger points may also manifest as tension headache, tinnitus, temporomandibular joint pain, decreased range of motion in the legs, and low back pain.”
As can be seen in the image below, multiple muscles of the neck and surrounding areas can develop trigger points referring pain to the head.
Primary vs. Secondary Headache
Primary headaches are headaches with no specific “known” cause, while secondary headaches, as you might have guessed, are caused by a primary source such as a blood vessel or injury to the neck.
The most common types of primary headaches are:
- Migraine
- Tension headache
- Cluster headache
The most common types of secondary headaches are:
- Cervicogenic (meaning it originates in the neck)
- Neuralgias (such as occipital, trigeminal, etc.)
Very uncommon secondary headaches:
- Space-occupying lesion
- Infection
- Vascular disease
Even though primary headaches don’t technically have a known cause, their origin can often be traced back to a most likely source.
You’ve guessed right, most can be traced back to an issue from the neck.
Muscles and Trigger Points
Authors of a paper published in Headache: The Journal of Head and Face Pain 3, in 2006, concluded that: “Active TrPs (Trigger Points) in upper trapezius, sternocleidomastoid, and temporalis muscles were associated with CTTH (Chronic Tension-Type Headaches). CTTH subjects with active TrPs usually reported a greater headache intensity and longer headache duration than those with latent TrPs. CTTH subjects with active TrPs tended to have a greater FHP than CTTH subjects with latent TrPs.”
Others found that: “Suboccipital active TrPs and FHP were associated with CTTH. CCTH subjects with active TrPs reported a greater headache intensity and frequency than those with latent TrPs. The degree of FHP correlated positively with headache duration, headache frequency, and the presence of suboccipital active TrPs.” in an article published in the journal Headache 4, in 2006.
These doctors also stated that “The degree of FHP was greater in CTTH subjects than in controls in both sitting and standing positions.”
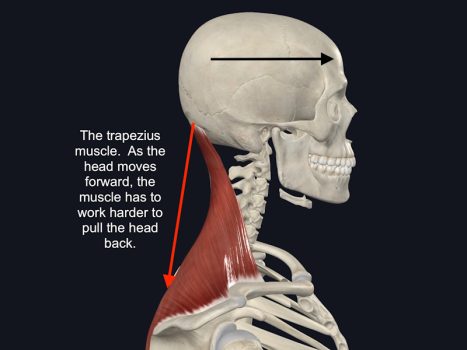
FHP increases load on the front of the spine, as the head moves further forward. This taxes the upper trapezius and suboccipital muscles, amongst others, as they are responsible for neck extension (bringing the head and neck back over the shoulders). Longstanding FHP is likely to create TrPts in the upper trapezius and suboccipital muscles.
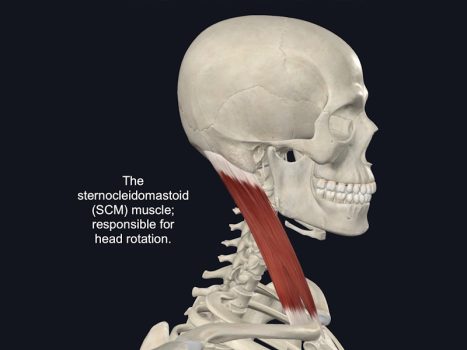
The sternocleidomastoid muscles’ main role is to rotate the head. Over 50% of head and neck rotation happens at the C1/C2 joints. The Atlas (C1), shaped like a donut, pivots on top of Axis (C2).
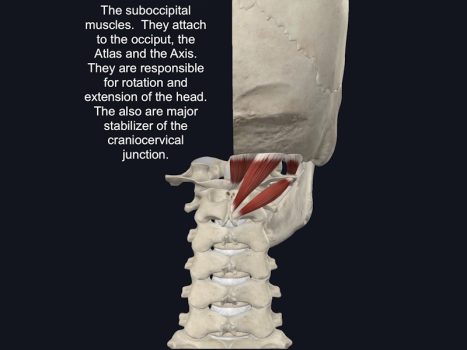
The suboccipital muscles are responsible for the rotation and extension of the head and neck.
If the Atlas is misaligned/malpositioned under the skulls and on top of the Axis, the rotation and extension, amid other ranges of motion, will be limited. When joints are misaligned, their surfaces don’t slide smoothly one on top of another. This can result in the common popping or crackling patients will mention. This lack of mobility, in the long run, will create tire tense muscles as they require more and more tension to create motion at the misaligned joints. Over time, trigger points will develop in the sternocleidomastoid and suboccipital muscles.
The temporalis is one of the 4 mastication muscles. It is located on the side of the head and helps close the jaw. The temporalis is innervated by the trigeminal nerve.
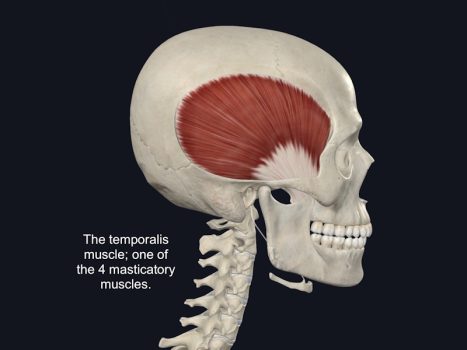
In our article “The missing link between TMJ dysfunction and the neck”, Dr. Felix writes:
We evaluate the head and neck of patients suffering from TMJ dysfunction because we are looking for indications of misalignment of the Atlas (C1), the neck, and the head. The head and neck area is weak and prone to injuries, and I commonly see structural issues with this area in patients suffering from dysfunction. Because of the close link between the neck and the jaw, one can cause issues to the other and vice versa.
When a dentist wants to fix a malocclusion problem it makes sense. Some occlusion treatments, that are gradual and reversible, can be extremely beneficial. However, many patients will only find partial relief from such a procedure until the problem with the alignment of their neck is resolved.
It’s also important to note that a problem with the alignment of the cervical spine (neck spine) is a common cause of all types of headaches including migraine, tension-type, cervicogenic, cluster, and thunderclap.
This has been known for a very long time hence why our evaluation always begins with a careful analysis of our patient’s head and neck.
A misalignment of the head and neck will have an effect on nerves and on the occlusion (the way teeth come together when the jaw closes down). Nerve dysfunction and malocclusion will both increase the risk of spasms in the temporalis leading to the formation of trigger points.
Let’s stop here for a recap.
- TrPts in the upper trapezius, sternocleidomastoid, and temporalis muscles are associated with CTTH.
- FHP is associated with suboccipital TrPts and CTTH
- A misalignment of the upper cervical spine will affect the joints of the spine; causing a decrease in mobility. This will in turn overwork the muscles of the head and neck resulting in TrPts.
- A misalignment of the upper cervical spine will change the center of gravity (point of balance) of the head, further increasing FHP; which will in turn create TrPts in the upper trapezius and suboccipital muscles. (*See section below: FHP and its Consequences*)
- A misalignment of the upper cervical spine will affect occlusion and the trigeminal nerve; both can lead to tension in the temporalis and the formation of TrPts
Muscle Connections of the
Upper Cervical Spine & Nerve Tissue
Recent cadaveric studies have aimed to better understand the very complex area of the craniocervical junction. One of the areas of study is the existence and relevance of myodural bridges. Myodural bridges are fascia (a type of soft tissue; similar to ligaments) connecting muscles to meningovertebral ligaments. In turn, these ligaments connect the dura (sheath around the spinal cord and brain) to ligaments stabilizing the spine. These findings indicate an indirect connection between muscle and nerve tissue.
The authors of a fascinating study from 2020, published in the journal PeerJ 5, wrote about their findings: “Myodural bridges: fascial connections between the Rectus Capitis Posterior Major, Rectus Capitis Posterior Minor, and the Obliquus Capitis Inferior and the dura have been demonstrated. Between the arches of C1 and C2, the myodural bridges merge with the meningovertebral ligaments and cross the epidural space, inserting into the posterior aspect of the dura mater.”
“The significance of this finding is that increased muscle tone might directly affect positioning of the dura in the spinal canal and it could be hypothesized that this might play a role in the development of cervicogenic headaches. A posterior pull of the dura can be expected with increased suboccipital muscle tone.”
They concluded by writing: “A suboccipital muscle contraction would result in a posterior pull on the dura through the myodural connections.” and “passive motion of the upper cervical spine and C1 results in a change of position of the spinal cord within the spinal canal and resulting in tightening of the myodural, meningovertebral ligaments, and spinal nerves.”
It is also important to point out the existence of the denticulate, or dentate, ligaments. These ligaments anchor the spinal cord to the spine, from the base of the skull to the beginning of the lumbar (lower back) spine. The dentate ligaments act as stabilizers; preventing excess motion of the spinal cord during movement of the spine.
Let’s stop for a quick recap:
- Myodural bridges connect suboccipital muscles to meningovertebral ligaments which connect the spinal cord to stabilizing ligaments of the neck
- Dentate ligaments connect vertebrae to the spinal cord
Now picture this. A misalignment of the Atlas; torquing the spinal cord via the dentate ligaments and tensing the suboccipital muscles, pulling on the spinal nerves. This is yet another example of the link between headaches and the neck.
Forward Head Posture (FHP)
and its Headache Consequences
As previously explored in the article “How the Neck Affects the TMJ”, FHP has multiple repercussions on the jaw and surrounding structures. As it relates to headaches, it should come to little surprise that FHP also plays a major role in their occurrence. The cervical spine and other closely related blood vessels, muscles, and nerves are affected by an anterior displacement of the head.
Indeed, researchers found that: “Loss of cervical lordosis leads to mechanical overload, structural degeneration, and reduced vertebral artery hemodynamics in the cervical region. However, the duration of headache attacks was longer in patients with loss of cervical lordosis.” as published in an article in the journal Medical Science Monitor 6, in 2023.
Another article reported that: “The meta-analysis showed that patients with chronic primary headache presented greater forward head posture than asymptomatic participants” 7.
As the head moves forward, further and further away from above the shoulders, its perceived (by the body) weight increases by 10 pounds for every inch. The heavy anterior weight will cause an abnormal load on the front part of the spine and a significant increase in muscle tension; in an attempt to pull the head back. As written above, FHP also affects on arteries; decreasing the blood flowing up to the brain.
One more article noted that: “In general, FHP leads to changes in the lengths of the anterior and posterior neck muscles, and prolonged FHP causes sustained loading on the cervical spine.” The researchers also write: “[…] changes in the lengths of muscles, as a result of FHP, have a bad influence on the activity of the muscle spindles […]” 8.
Muscle spindles respond to a stretch in a muscle by causing a contraction. Long-term elongation or shortening of a muscle, by gross change in spinal curvature, can lead to a decrease in muscle activity or spams in others.
Other researchers also write: “An important contribution of the cervical spine is its role in the maintenance of human posture and balance. A greater contribution is attributed to the upper cervical spine since it contains most of mechanoreceptors and muscle spindles connected with visual, vestibular and sympathetic systems to provide proper proprioception” 9.
Both mechanoreceptors and muscle spindles are extremely sensitive to a misalignment, however small it could be, because of the importance of the area for balance, posture and vision.
Neuromusculoskeletal
Neck Problems, Headaches, & Migraines
There is a very strong association between migraines and the neck. This is due, largely, because of the connection the upper cervical spine, its nerves, and the trigemino-cervical nucleus have together.
Researchers from Europe write: “Musculoskeletal disorders in the cervical spine may contribute to migraine pain by sensitization of trigemino-cervical nucleus caudalis, the anatomical area where nociceptive afferent inputs from the upper cervical roots (C1-C3), the first division of the trigeminal nerve, and cranial dura converge.” 9.
Nociception is the fancy medical word for “pain.” The word afferent means “information going from the body to the brain. In summary, what the above statement means is this: problems of the neck spine may contribute to migraine by increasing the sensitivity of the trigemino-cervical nucleus caudalis (which is located, by the way, at the level of the junction between the skull and the Atlas); the area where the pain signals from the upper cervical nerves, a branch of the trigeminal nerve and the nervous tissue covering the brain converge.
Published in the Journal of Physical and Rehabilitation Medicine, in 2017, the article ends with a conclusion stating: “Women with migraine exhibit musculoskeletal impairments of the upper cervical spine expressed as restricted cervical rotation, decreased upper cervical rotation, and the presence of symptomatic upper cervical joints.”
These findings fully correlate with, you guessed it, a misalignment of the Atlas.
Researchers from Brazil published in 2016, in the Journal of Electromyography and Kinesiology 10, some interesting findings concerning changes in muscles and migraine. They concluded that: “[…] women with chronic migraine exhibit increased activity of their superficial neck extensor muscles when acting as antagonists during low-load isometric CCF (craniocervical flexion) contractions in comparison to non-headache subjects.”
This denotes a dysfunction with the cervical spine motions and muscle action. As the neck flexes (the head moving forward and downward), it is expected that the muscles of the back of the neck activate to control the motion. However, the difference with the non-headache group could be attributed to an instability of the cervical spine, FHP, and/or a misalignment of the upper cervical spine.
Lastly, a paper published in the journal Physical Therapy 11, in 2019, concluded by stating: “[…] there are indeed detectable musculoskeletal changes in patients with migraine, which can be assessed and quantified. […] the recommended tests for this purpose are cervical range-of-motion testing in extension and rotation, the flexion-rotation test, evaluation of the forward head posture in standing […].”
The flexion-rotation test is specifically used to isolate and assess the normalcy of the upper cervical spine. Limited ranges of motion and FHP are also primary indicators of a misalignment of the craniocervical junction.
Overall, we can extract from the above these facts:
- Dysfunction of the upper cervical spine will cause an increase in sensitivity of the pain-receiving nerves of the head, neck and face.
- Migraine sufferers have an increased tension in tension of the muscle of the back of the head.
- A malfunctioning cervical spine, in alignment and motion, is associated with migraine.
Compression of the Occipital Nerves,
Occipital Headaches, & Occipital Neuralgia
Occipital neuralgia (ON) is a secondary headache originating from the severe compression and irritation of one or more occipital nerves. Simple occipital nerve compression is far more common and presents with lighter symptoms such as: pressure and tightness at the base of the skull. Occipital neuralgia generally presents with throbbing, sharp, shooting pain starting at the base of the skull and traveling across the back of the head; pain behind an eye is also common. 3 occipital nerves can cause this painful condition: the Greater Occipital Nerve (GON), the Lesser Occipital Nerve (LON), and the 3rd Occipital Nerve.
The GON and LON are the most often affected nerves. Compression of these nerves is frequently due to the muscles they pierce as they leave the spinal cord, travel in between the upper cervical vertebrae and the base of the skull, on their way to the back of the scalp.
In an article published in The Journal of Headache and Pain 12, in 2019, researchers from the University of Texas and Harvard Medical School wrote:
We hypothesize that anatomic entrapment of the GONs and LONs occurs as the nerves pierce the muscular structures of the posterior neck and the fascial attachments at the occipital ridge. […] subsequent inflammation develops over time due to axonal compression as well as ischemia of the peripherally placed nerve vasculature, and perhaps intensified by other factors such as trauma in the form of either a direct blow or intense pressure to the occiput, or a stretch injury of the nerves. We further speculate that the combination of progressive inflammation with additional direct compression of the nerve by the accumulating inflammatory tissue and spasm in the surrounding muscle leads to unremitting pain in the suboccipital area of the neck and the occiput, which may also radiate to more distal distributions of the occipital nerves at the vertex or temples. Comorbid symptoms including occipital allodynia and pain and painful spasms in cervical and trapezius muscles may also develop.
The problem of muscle spasms is regularly associated with all kinds of headaches. In the case of occipital nerve compression and occipital neuralgia, suboccipital muscles appear to be the generally accepted culprits. Nonetheless, we cannot forget the possibility of vertebral compression at the junction between the occiput-C1 and C1-C2. Cadaver studies point to the possibility that “the underlying pathophysiology of the headaches associated with FHP is poorly understood and is likely multifactorial. One possible component may be compression of the Greater Occipital Nerve (GON) or C2 nerve root (C2nr) within the Suboccipital Triangle (SOT)” 13.
Lastly, published in the Pain Physician journal 14, in 2000, an article points to the very important aspect of occipital pain arising from upper cervical spine joints. Indeed, they write:
Pain arising from inflammation of the upper cervical spine joints, namely, the atlanto-occipital and atlanto-axial joints, respectively, typically presents with occipital headaches, which are often associated with suboccipital pain and aggravated by lateral rotation of the cervical spine and/or flexion or extension of the cervical spine. […] It is important to note that occipital headaches can arise from injuries affecting the disc of the C2-3, as well as its facet joints and the atlantoaxial and atlanto-occipital joints.
Just as in the research explored above, they reiterate the involvement of the occipital nerves writing: “The atlas and axis do not have intervertebral foramina. The C1 and C2 nerves, which are primarily sensory, travel through muscle and fascia to the occipital area as the greater occipital nerves and the lesser occipital nerves.”
The Effects of an
Atlas Spinal Misalignment (ASM)
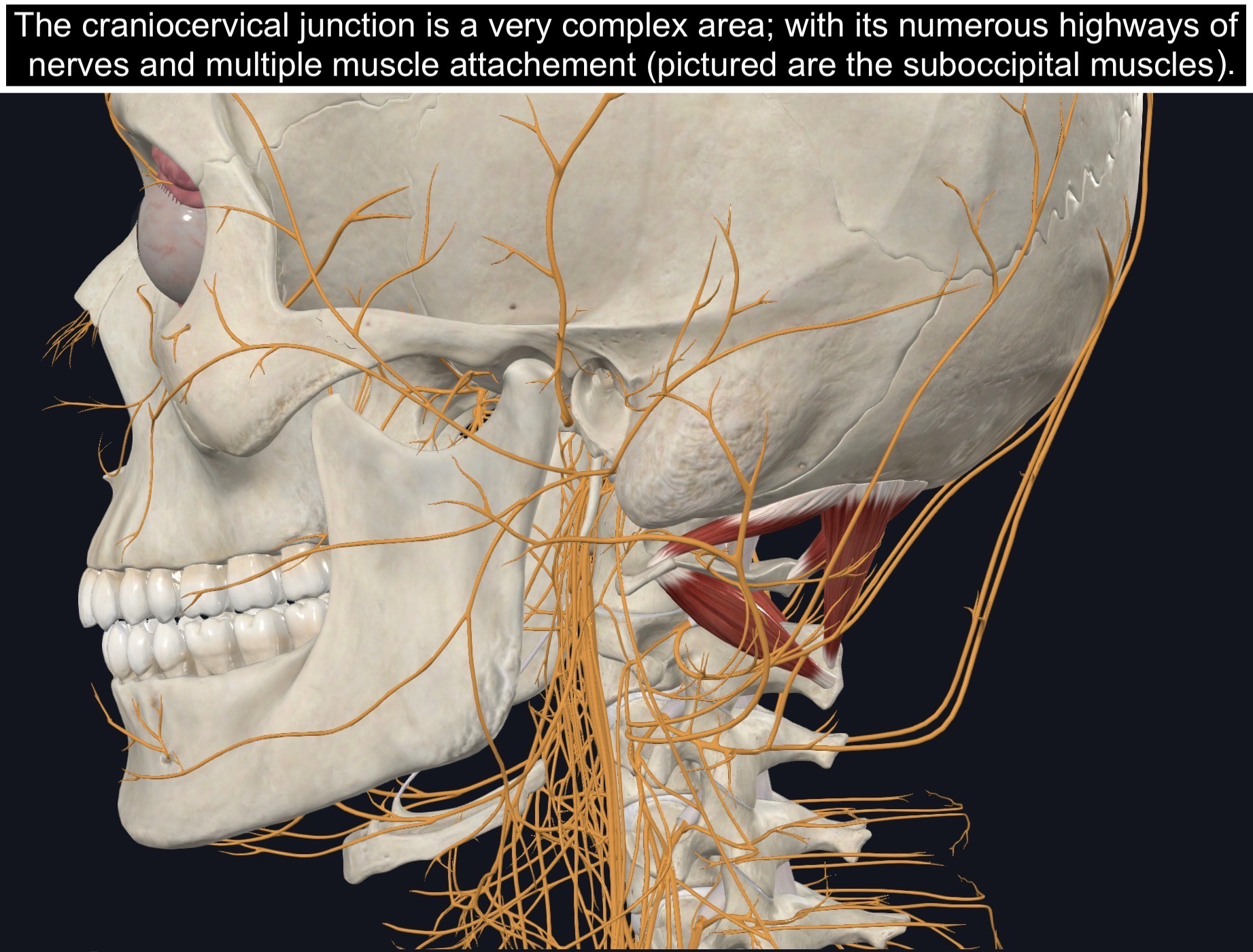
The upper cervical spine is one of the most complex regions of the body. It is the junction point between a very heavy ball (namely the head) and a very tiny bone. It is also the junction between the brain and its continuation downstream as the brainstem and spinal cord. Although there are numerous structures essential for life, this part of the spine is the most delicate.
Mobility is crucial to all living beings and humans are certainly part of this category. The incredible range of motion the neck allows (think about how much you can look around) comes at a high price; its instability and delicateness. In an attempt to maximize stability while keeping mobility, the human machine was designed with several muscles and ligaments to accomplish this difficult task.
Taking all this into account, it comes as no surprise that something can go utterly wrong if and when the upper cervical spine is compromised.
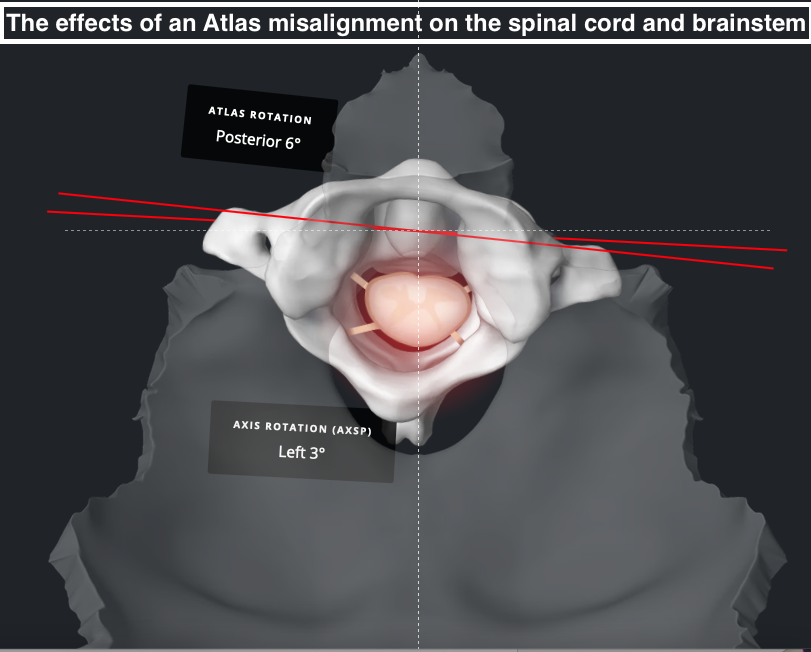
This is the picture-perfect visual of an Atlas Spinal Misalignment. It is obvious to see how the skull is tilted to the right, the Atlas shifted and elevated to the left and the entire neck leaning to the left.
A misalignment of the upper cervical spine, where the Atlas loses its normal relationship and balance with the skull, above, and the neck, below; will cause a wide array of consequences.
First, the nerve problem: an Atlas Spinal Misalignment will cause dysfunction of spinal and cranial nerves. Possibly by direct compression as is the case with the vagus nerve and occipital nerves. Possibly by tension as is the case with the dentate ligaments; or even because of sensitization of the trigemino-cervical nucleus.

Secondly, the joint problem: an ASM, because of its inherent shift in normal spinal alignment, will cause uneven pressure on the structure; namely the joints (including the intervertebral discs). The stress will result in joint malfunction and inflammation; presenting as decrease ranges of motion, referred pain and, visually, arthritis.
Tertiary, the muscle problem: an abnormal position (alignment) of the spine, as seen in cases of an ASM, will undoubtedly create unequal muscle tone. With time, the abnormality in muscle tissue leads to spasms. *It is important here to understand that a spasm doesn’t have to be dramatic as in a hamstring of foot cramp. Those are certainly spasms, but the muscular system can also suffer a “low-grade spasm,” one that is not as perceptible as a full-on cramp.* These spasms can turn into TrPts, causing referred pain to the head and/or neck. They can also cause tension on ligaments, themselves tensioning on nerves. Finally, muscles can compress nerves as is the case with the occipital nerves (the sciatic nerve is another example; this one, sometimes compressed by the piriformis muscle).
Lastly, the ligament problem: an ASM, with its shift in structural alignment, comes with the consequence of ligament stretch. Over time, this stretch on ligaments can cause instability, which worsens all previous problems. An injured C2-C3 disc can cause referred pain. And just as written above, dentate ligaments and meningovertebral ligaments can pull on nerves as a result of a misaligned upper cervical spine.
Summary
There is indeed a very strong connection between the neck and headaches. Muscles, ligaments, nerves, bones (vertebrae) and even blood vessels can all factor into a headache problem.
The main nucleus of all these problems seems to come back to the spine; more specifically the upper cervical spine. With its numerous muscle attachments, ligament connections, nerves in very close proximity; and direct links to the spinal cord, the craniocervical junction, without surprise, plays an immense role in the onset and persistence of headaches.
TrPts in muscles as well as joints of the cervical spine can refer pain to the head. Ligaments can pull on muscles and nerve structures, thus causing a muscle problem, on one hand, and/or a nerve dysfunction, on the other.
The Atlas, if misaligned, has the potential to imbalance the entirety of the head and neck relationship; and all structures usually in harmony, with the area. This is the biggest problem I know of. A problem capable of causing dysfunction of nerves, especially the trigemino-cervical nucleus; a problem capable of creating TrPts and tension on ligaments; and a problem capable of causing uneven load on cervical spine joints, referring pain to the head and/or neck.
Headache Treatment
We commonly hear patients talk about neck problems with headaches. We evaluate the head, neck, and Atlas of all patients coming to our clinic suffering from headaches. We look for signs and symptoms of joint compression, muscle spasms, ligament pull, and nerve dysfunction. We take unique X-rays proprietary to the NUCCA and Atlas Orthogonal techniques to analyze, qualify and quantify the ASM. Doing so allows us to have a detailed understanding of the structure of the head and neck, their malposition, and specifically what to do to correct this misalignment.
Once the X-rays are taken and analyzed, the ASM can be corrected, or at least reduced. This in turn brings the head and neck back to a normal and stable relationship. Sometimes instantaneously, others, with time, the headaches reduce and often completely disappear; as long as the ASM stays in its correct position.
The correction of the ASM is gentle and painless, which is why it can last for much longer than any other forms of adjustments/manipulation. It also causes zero damage to the anatomy of the head and neck, as compared to very forceful therapy done to the neck.
To learn more about the ASM and our process of correcting it, you can read more here🔗.
If you’re interested in having your own evaluation, you can schedule a consultation with Dr. Felix Periard with the button below!
References
- Martínez Barbero JP, Láinez Ramos-Bossini AJ, Rivera-Izquierdo M, Sendra-Portero F, Benítez-Sánchez JM, Cervilla JA. Prevalence and Risk Factors Associated with Tumors and Other Structural Anomalies in Brain MRI Performed to Rule out Secondary Headache: A Multicenter Observational Study. Int J Environ Res Public Health. 2022 Mar 16;19(6):3521. doi: 10.3390/ijerph19063521. PMID: 35329206; PMCID: PMC8956087.
- Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. Am Fam Physician. 2002 Feb 15;65(4):653-60. PMID: 11871683.
- Fernández-de-Las-Peñas C, Alonso-Blanco C, Cuadrado ML, Gerwin RD, Pareja JA. Myofascial trigger points and their relationship to headache clinical parameters in chronic tension-type headache. Headache. 2006 Sep;46(8):1264-72. doi: 10.1111/j.1526-4610.2006.00440.x. PMID: 16942471.
- Fernández-de-las-Peñas C, Alonso-Blanco C, Cuadrado ML, Gerwin RD, Pareja JA. Trigger points in the suboccipital muscles and forward head posture in tension-type headache. Headache. 2006 Mar;46(3):454-60. doi: 10.1111/j.1526-4610.2006.00288.x. PMID: 16618263.
- Sillevis R, Hogg R. 2020. Anatomy and clinical relevance of sub occipital soft tissue connections with the dura mater in the upper cervical spine. PeerJ 8:e9716 DOI 10.7717/peerj.9716
- Delen V, İlter S. Headache Characteristics in Chronic Neck Pain Patients with Loss of Cervical Lordosis: A Cross-Sectional Study Considering Cervicogenic Headache. Med Sci Monit. 2023 Mar 14;29:e939427. doi: 10.12659/MSM.939427. PMID: 36915178; PMCID: PMC10024460.
- Elizagaray-Garcia I, Beltran-Alacreu H, Angulo-Díaz S, Garrigós-Pedrón M, Gil-Martínez A. Chronic Primary Headache Subjects Have Greater Forward Head Posture than Asymptomatic and Episodic Primary Headache Sufferers: Systematic Review and Meta-analysis. Pain Med. 2020 Oct 1;21(10):2465-2480. doi: 10.1093/pm/pnaa235. PMID: 33118601.
- Lee MY, Lee HY, Yong MS. Characteristics of cervical position sense in subjects with forward head posture. J Phys Ther Sci. 2014 Nov;26(11):1741-3. doi: 10.1589/jpts.26.1741. Epub 2014 Nov 13. PMID: 25435690; PMCID: PMC4242945.
- Ferracini GN, Florencio LL, Dach F, Bevilaqua Grossi D, Palacios-Ceña M, Ordás-Bandera C, Chaves TC, Speciali JG, Fernández-de-Las-Peñas C. Musculoskeletal disorders of the upper cervical spine in women with episodic or chronic migraine. Eur J Phys Rehabil Med. 2017 Jun;53(3):342-350. doi: 10.23736/S1973-9087.17.04393-3. Epub 2017 Jan 24. PMID: 28118694.
- Florencio LL, Oliveira AS, Lemos TW, Carvalho GF, Dach F, Bigal ME, Falla D, Fernández-de-Las-Peñas C, Bevilaqua-Grossi D. Patients with chronic, but not episodic, migraine display altered activity of their neck extensor muscles. J Electromyogr Kinesiol. 2016 Oct;30:66-72. doi: 10.1016/j.jelekin.2016.06.003. Epub 2016 Jun 9. PMID: 27317975.
- Szikszay TM, Hoenick S, von Korn K, Meise R, Schwarz A, Starke W, Luedtke K. Which Examination Tests Detect Differences in Cervical Musculoskeletal Impairments in People With Migraine? A Systematic Review and Meta-Analysis. Phys Ther. 2019 May 1;99(5):549-569. doi: 10.1093/ptj/pzz007. PMID: 30690564.
- Blake, P., Burstein, R. Emerging evidence of occipital nerve compression in unremitting head and neck pain. J Headache Pain 20, 76 (2019).
- Olivia A. Kalmanson, Saeed Khayatzadeh, Anand Germanwala, Matthew Scott-Young, Robert M. Havey, Leonard I. Voronov, Avinash G. Patwardhan, Anatomic considerations in headaches associated with cervical sagittal imbalance: A cadaveric biomechanical study, Journal of Clinical Neuroscience, Volume 65, 2019, Pages 140-144, ISSN 0967-5868
- Ogoke BA. The management of the atlanto-occipital and atlanto-axial joint pain. Pain Physician. 2000 Jul;3(3):289-93. PMID: 16906186.
